ASD and Gut Imbalance: Microbes in Quicksand By MSC Susana Reyes
Homo sapiens’ entities are the overwhelming minority in our bodies: there are 10 times more microbial cells than human cells. Across centuries, we’ve learned not only to coexist but to strive towards the goal of mutual survival. However, as microbial populations shuffle in type and population across different tissues of our bodies we are prone to experience maladaptation consequences. The microbial population in each tissue is often referred to as the microbiome.
The gut is one of the most studied human surfaces known to have a rich and extensive microbiome. The gut, through the intestinal wall, comprises a physical selective barrier that allows nutrients and bacterial metabolites to be absorbed and transported to the bloodstream to hungry and developing tissues around the body. If the intestinal wall is disrupted, behaving a little bit like quicksand, then bigger molecules than usual could pass through this barrier, be recognized as potential threats, and activate a defensive response by the immune system such as food allergies.
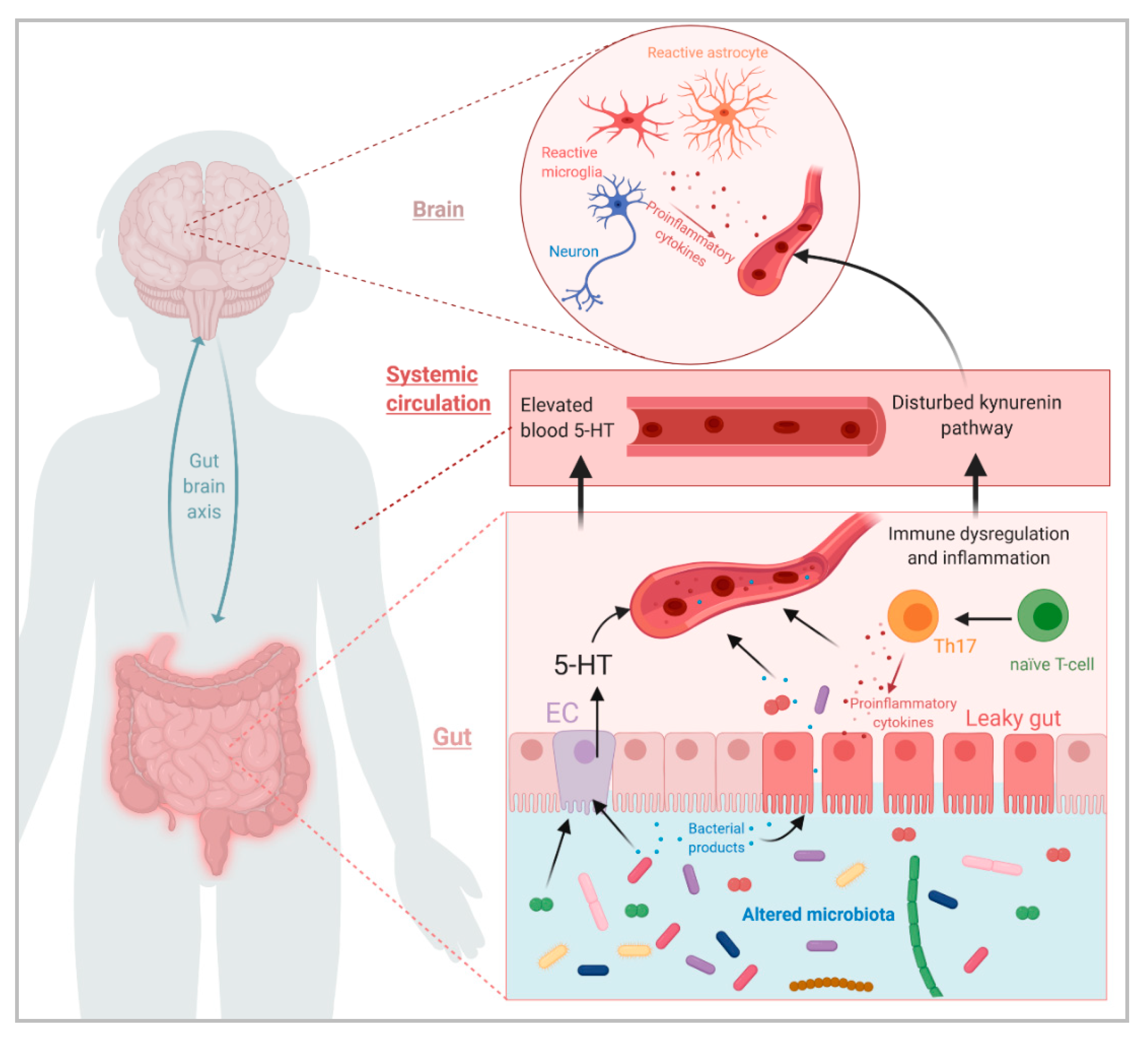
Increased gut permeability, or leaky gut, also allows bacterial molecules to cross the barrier and potentially alter brain development during early childhood in susceptible individuals.
Autism Spectrum Disorder (ASD) patients, almost half of children with ASD, report at least one gastrointestinal symptom with diarrhea and constipation being the most common symptoms presented[1-3]. Also, studies have shown that the severity of gastrointestinal symptoms is significantly correlated with the severity of ASD symptoms[4-6]. These gastrointestinal disturbances may be associated with an imbalance gut microbiome and increased gut permeability.
The microbiome composition in ASD patients has been found to be less diverse than neurotypical individuals. Gut bacteria help process sugars and fats from the diet, and when this equilibrium is disrupted the intestinal wall may sacrifice its integrity and be more prone to inflammation.
A more permeable gut allows bacterial molecules and environmental toxins and environ to freely cross the intestinal barrier and potentially modify neuronal activity. This gut-brain axis is crucial to understand how the gastrointestinal system is not just a digestive tract, but also a route by which human cells communicate with environmental factors resulting in particular immunological and neurological features.
References.
- Holingue C, Newill C, Lee LC, Pasricha PJ, Daniele Fallin M. Gastrointestinal Symptoms in autism Spectrum Disorder: a review of the literature on ascertainment and prevalence. Autism Res. 2017; 11:24-36.
- Thylasi V, Steer RA, Monteiro IM, Ming X. Overall severities of gastrointestinal symptoms in pediatric outpatients with and without Autism Spectrum Disorder. Autism. 2018.
- Chaidez V, Hansen RL, Hertz-Picciotto I. Gastrointestinal problems in children with autism, developmental delays or typical development. J Autism Dev Disord. 2013. 44:1117-27.
- Adam JB, Johansen LJ, Powell LD, Quig D, Rubin RA. Gastrointestinal flora and gastrointestinal status in children with autism- comparisons to typical children and correlation with autism severity. BMC Gastroenterol. 2011. 11:22.
- Tomova A, Husarova V, Lakatosova S, et al. Gastrointestinal microbiota in children with autism in Slovakia. Physiol Behav. 2015. 138:179-87.
- Gorrindo P, Williams KC, Lee EB, Walker LS, McGrew SG, Levitt P. Gastrointestinal dysfunction in autism: parental report, clinical evaluation, and associated factors. Autism Res. 2012. 5:101-8.
- Fowlie G, Cohen N, Ming X. The perturbance of microbiome and gut-brain axis in Autism Spectrum Disorders. Int J Mol Sci. 2018. 19(8):2251.